Hospice Advisors Case Study
Title: Building Strategic Partnerships With Senior Living Communities
Company: A Hospice Company located in Texas
Date: December 22, 2014
Problem: Too many chiefs in the kitchen!
Presenting Issues/Challenges: This is a case where I assisted a hospice collaborate with a “super-SNF” to create a partnership between hospice, home care and personal care companies. This specific “super-SNF” had 11 hospice companies, 13 skilled home care companies and 9 personal care home health companies working this facility for referrals. There was too much variation in the care delivered and an inability to track and gather outcome data!
Plan of Action: The executive in this facility made a bold move. He told all the hospices, home care, etc. that he would be selecting only 3 providers from each group (home care, etc.) to be part of this facilities team. Other providers would be allowed in the building if they had a patient that came to his building from another location like a hospital. Otherwise, the partnership team would work together to care for residence and patients being admitted to the facility. The executive sent out a “mini Request For Proposal” to create a process by which to select three partners from each provider group.
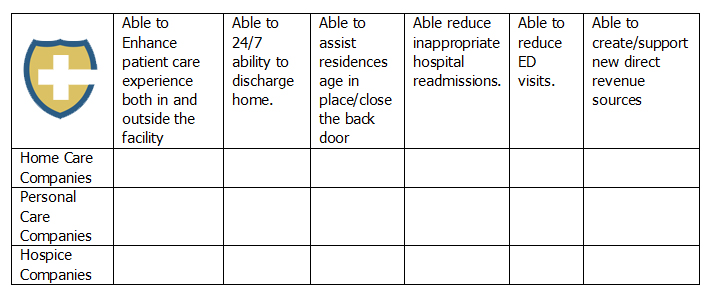
The chart at the end of this case is a value proposition matrix the executive from the “super-SNF” used to identify companies that would bring the most value, while also providing a great partnership.
Three hospice, home care and personal care companies were selected.
Outcome/Results:
1. Worked together to reduce unnecessary ER visits and inappropriate hospital re-admissions.
When the team could, they looked for opportunities to avoid an emergency department visit and sent appropriate patients directly to one of the “team” members. Home care, personal care, and hospice companies worked creatively to keep patients safe and secure in the home setting.
If a patient did go to the ER, the team worked diligently to send them right back allowing that company to better manage their care. If the patient was a fall risk, a personal care referral was made. If the patient met hospice eligibility guidelines, the appropriate referral was made.
2. Developed a general inpatient (GIP) hospice program.
The hospice I worked for approached the executive from the “super-SNF” to develop a GIP cluster bed program. This was an excellent development of a program element that greatly improved the “super-SNF” ability to reduce re-admissions and create a new revenue stream.
This was accomplished by turning two beds at the end of a wing into palliative care suites. For patients in the community that met GIP criteria, they were cared for in one of these palliative care suites to treat and get their breakthrough pain or out of control symptoms under control. This helped make a discharge home more manageable.
Instead of going to the hospital, those patients discharged home who developed GIP related issues could be admitted to the palliative care suite for care. All appropriate care was handled by the team, and the facility was reimbursed $375 per day from the hospice for the use of the bed and facility’s services. The GIP level of care is allowed and encouraged by CMS. Ultimately this provided the community the ability to generate $260,000 in one year from the hospice providing GIP care, in addition to driving better outcomes.
3. Data Tracking: One of the final steps was data tracking.
The “super-SNF” monitored the team members as well as physicians’ data and compliance through benchmarking.
This facility started to share the data with hospitals, which resulted in the facility becoming part of a hospital’s post-acute provider networks. This benefited all the members of the “team” and allowed the facility to customize their data, and actually provided more information than is often requested to help create a clear picture of the efforts and results.
4. Personal Care Services.
The partnership with the personal care company was creatively used in a number of ways. One example is how a small office space was given to the three personal care companies that rotated its use, so that a caregiver was on the campus seven days a week, 10 hours per day. The personal care company paid for this staffing and, in part, the caregiver would provide a number of services such as helping with discharges home, assisting with transportation home (if needed), and providing three hours of “tuck-in” service at home. This safe discharge home program was paid for either by the family or the facility.
5. Hospice Established as a Thought Leader.
The hospice was the company that helped facilitate the creation of this partnership. Because of that was viewed as a thought-lead.